Exploring the Link Between Viruses and Neurological Diseases: Epstein–Barr Virus and Beyond
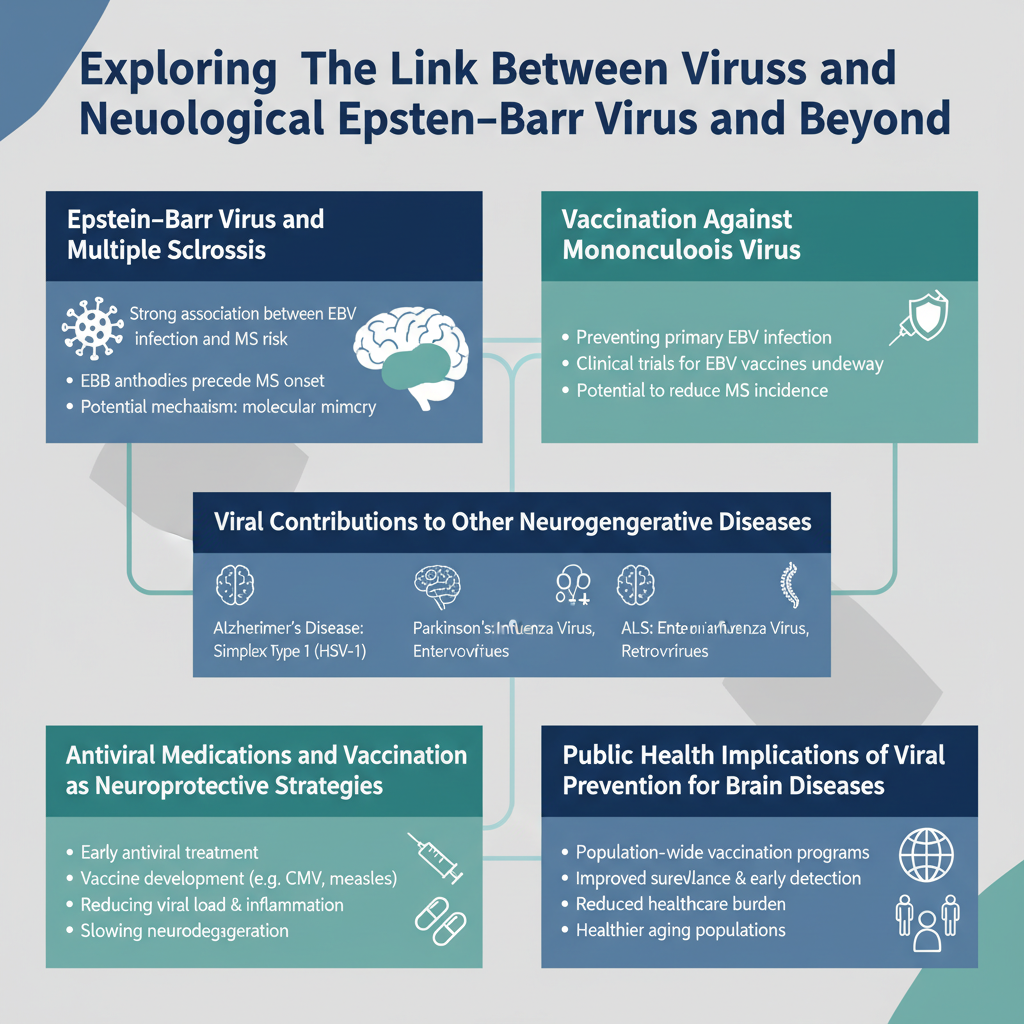
Recent studies highlight a strong connection between viral infections—especially the Epstein–Barr virus (EBV)—and neurological diseases such as multiple sclerosis (MS), Alzheimer’s, Parkinson’s, and ALS. Nearly all MS patients have prior EBV infection, suggesting the virus may trigger the disease through immune mechanisms. Vaccination against EBV, currently in development, holds promise to reduce MS incidence by preventing mononucleosis. Moreover, chronic neuroinflammation induced by various viruses may contribute to other neurodegenerative conditions. Antiviral treatments and vaccines, including the shingles vaccine, are being explored for their neuroprotective potential. Public health strategies focusing on viral prevention could significantly lower the burden of these brain diseases, representing a pivotal shift in how we approach neurodegeneration prevention and therapy.
Summary
Exploring the Link Between Viruses and Neurological Diseases: Epstein–Barr Virus and Beyond
Recent research has revealed compelling connections between viral infections—particularly the Epstein–Barr virus (EBV)—and the development of various neurological disorders such as multiple sclerosis (MS), dementia, Alzheimer's disease, Parkinson’s disease, and amyotrophic lateral sclerosis (ALS). Understanding these associations offers promising avenues for prevention through vaccination and antiviral treatments, potentially reducing the overall burden of neurodegenerative diseases globally.
- Epstein–Barr virus infection is strongly linked to the development of multiple sclerosis.
- Vaccination against EBV could significantly lower the incidence of MS by preventing mononucleosis.
- Chronic neuroinflammation triggered by viral infections may contribute to Alzheimer’s, Parkinson’s, and ALS.
- Antiviral medications and vaccines, including the shingles vaccine, are being investigated for neuroprotective effects.
- Public health strategies focusing on viral prevention could reduce the prevalence of various brain diseases.
Epstein–Barr Virus and Multiple Sclerosis: An Emerging Causal Relationship
The Epstein–Barr virus, a member of the herpesvirus family, is best known for causing infectious mononucleosis, commonly called "mono." Epidemiological studies have consistently shown that nearly all individuals diagnosed with multiple sclerosis have previously been infected with EBV, suggesting a strong link between the virus and MS pathogenesis.
Evidence Supporting EBV as a Trigger for MS
- Serological Studies: Elevated antibodies against EBV antigens are found in individuals before MS onset, indicating prior infection.
- Temporal Link: The age at EBV infection correlates with MS risk; delayed infection during adolescence or adulthood increases the likelihood of developing MS.
- Molecular Mimicry: EBV proteins may resemble components of the central nervous system, leading to an autoimmune response that damages myelin sheaths protecting nerve fibers.
These findings have led researchers to propose that preventing EBV infection through vaccination could dramatically reduce new MS cases.
Vaccination Against Mononucleosis Virus: A Potential Strategy to Prevent MS
Currently, no vaccines are licensed specifically to prevent EBV infection. However, candidates are in clinical development stages, aiming to prevent mononucleosis and potentially lower long-term MS risk.
Implications of EBV Vaccination
- Reducing MS Incidence: By blocking primary EBV infection, vaccination could eliminate the viral trigger implicated in MS.
- Lowering Healthcare Burdens: Decreasing MS cases would reduce disability and healthcare costs associated with chronic neurological disease management.
- Broadening Vaccine Targets: Efforts include vaccines targeting other herpesviruses to prevent associated neurological complications.
Viral Contributions to Other Neurodegenerative Diseases
Beyond EBV and MS, research is increasingly indicating that various viruses may play roles in the onset or progression of diseases like Alzheimer's, Parkinson’s, ALS, and dementia through chronic neuroinflammation.
Neuroinflammation as a Common Pathway
- Viral infections can activate immune cells in the brain, causing persistent inflammation.
- This chronic neuroinflammation damages neurons and disrupts normal brain function.
- Examples include herpes simplex virus (HSV) in Alzheimer's pathology and human immunodeficiency virus (HIV)-associated neurocognitive disorders.
Parkinson’s Disease and Viral Links
- Some studies suggest that viral infections may trigger the degeneration of dopamine-producing neurons.
- Influenza virus and other pathogens have been investigated for their role in triggering Parkinsonian symptoms.
ALS and Viral Hypotheses
- Though less established, viral infections may contribute to motor neuron degeneration in ALS through immune-mediated mechanisms.
Antiviral Medications and Vaccination as Neuroprotective Strategies
Given viral contributions to neurological diseases, antiviral therapies and vaccines are under investigation as potential preventive or disease-modifying treatments.
Shingles Vaccine and Neuroprotection
- The shingles vaccine, effective against varicella-zoster virus, has been associated with reduced incidence of dementia in some observational studies.
- It is hypothesized that preventing herpesvirus reactivation helps reduce neuroinflammation and subsequent cognitive decline.
Broad-Spectrum Antiviral Approaches
- Ongoing research explores antiviral compounds targeting EBV and other neurotropic viruses.
- Successful treatments could slow disease progression or prevent onset in high-risk individuals.
Public Health Implications of Viral Prevention for Brain Diseases
Vaccination programs have historically reduced the burden of infectious diseases; expanding this success to neurological diseases carries significant public health promise.
- Prioritizing EBV vaccine development could transform MS prevention.
- Educating clinicians and the public about viral risk factors for neurodegeneration is essential.
- Integrating antiviral therapy into neurological disease management protocols may improve patient outcomes.
Conclusion
The accumulating evidence that viruses—particularly Epstein–Barr virus—play a causal role in neurological diseases marks a paradigm shift in understanding and preventing these conditions. Vaccination against EBV and other neurotropic viruses, along with antiviral medications, represents a promising frontier in reducing the incidence and severity of disorders like multiple sclerosis, Alzheimer’s disease, Parkinson’s disease, and ALS. Continued research and public health initiatives targeting viral prevention could substantially alleviate the societal and individual impacts of neurodegenerative diseases in the coming decades.
Frequently Asked Questions
Q: are viruses causing neurological diseases
A: Yes, certain viruses can cause neurological diseases by infecting the nervous system. Examples include the herpes simplex virus, which can cause encephalitis, and the rabies virus, which affects the brain and spinal cord. Viral infections can lead to inflammation, nerve damage, and other neurological symptoms. These conditions may range from mild to severe and sometimes require prompt medical treatment.
Q: link between Epstein–Barr virus and multiple sclerosis
A: Research suggests a strong association between Epstein–Barr virus (EBV) infection and the development of multiple sclerosis (MS). EBV, a common herpesvirus, is thought to trigger abnormal immune responses that may contribute to MS, an autoimmune disease affecting the central nervous system. Studies show that people with prior EBV infection have a higher risk of developing MS, although the virus alone does not cause the disease. The exact mechanism linking EBV to MS remains under investigation.
Q: effect of shingles vaccine on Alzheimer's risk
A: Recent studies suggest that receiving the shingles vaccine may be associated with a reduced risk of developing Alzheimer's disease. The vaccine helps prevent shingles and its complications by boosting the immune response against the varicella-zoster virus, which some research links to neurodegeneration. While the exact mechanism is not fully understood, vaccination might lower inflammation or viral triggers involved in Alzheimer's progression. However, more research is needed to confirm the protective effect and understand how significant this impact might be.
Q: new treatments for MS involving antivirals
A: Multiple sclerosis (MS) is primarily managed with immunomodulatory therapies, but some research has explored antiviral treatments given speculation that viruses such as Epstein-Barr virus (EBV) may trigger MS. New approaches include experimental antiviral drugs targeting EBV to reduce its activity, potentially slowing MS progression. Clinical trials are ongoing to evaluate the safety and effectiveness of these antivirals in MS patients. However, antiviral treatments are not yet standard therapy for MS and remain under investigation.
Q: research on viral causes of Parkinson's and dementia
A: Research into viral causes of Parkinson's disease and dementia explores the hypothesis that certain viral infections may contribute to the development or progression of these neurological disorders. Some studies suggest that viruses like influenza, herpes simplex, or human immunodeficiency virus (HIV) may trigger inflammatory or immune responses in the brain, potentially leading to neuronal damage. However, direct viral causation remains unclear, and more research is needed to establish definitive links and mechanisms. Overall, understanding viral influences could open new avenues for prevention and treatment.
Key Entities
Øivind Torkildsen: Øivind Torkildsen is a neurologist at Haukeland University Hospital and a professor at the University of Bergen's Department of Clinical Medicine. He also serves as head of the Section for Neurology at the University of Bergen.
Charalampos Tzoulis: Charalampos Tzoulis is a Professor of Neurology and Neurogenetics at the University of Bergen and Haukeland University Hospital. He is internationally recognized for his research on movement disorders and neurodegenerative diseases.
Haukeland University Hospital: Haukeland University Hospital in Bergen, Norway, is the largest hospital in the country by number of patients and serves as a regional hospital for Vestland and Rogaland counties. It plays a significant role in medical care and research within the Bergen Hospital Trust.
University of Bergen: The University of Bergen is a public research university established in 1946 in Bergen, Norway. It offers diverse academic programs with over 20,000 students and is noted for its faculty of psychology and legal studies.
Moderna: Moderna, Inc. is an American biotechnology company based in Cambridge, Massachusetts, specializing in mRNA therapeutics and vaccines. It developed one of the earliest COVID-19 vaccines authorized for emergency use in the United States.
Relaterte artikler
Health